Axumin (18Fluciclovine) is a radiopharmaceutical that is proving to be a game-changer, particularly in the field of prostate cancer detection.
Previously, clinicians in the U.S. had little choice but to use 18FDG to perform the majority of PET/CT imaging. This has some major limitations for prostate imaging, such as bladder interference and a reliance on physical changes within the body to get results from imaging.
Axumin allows healthcare providers to image cellular activity and provides the best of both worlds for soft tissue and bone imaging. Here we’re looking at the clinical impact of using it in your practice:
Background on Axumin (18Fluciclovine)
Up to one-third of men that have had treatment for primary prostate cancer experience a biochemical recurrence within 10 years. Within that population, one-third will develop metastases within 8 years.
Typically, detection of prostate cancer recurrence has relied upon PSA (prostate-specific antigen) levels and limited information that can be provided by MRI and ultrasound examinations.
Limitations of current imaging procedures include:
- Low detection rates: Positive findings occur in only ~11% of patients with biochemical recurrence.
- Small tumors may not be detected: Some imaging procedures may be unable to detect recurrent prostate tumors <1 centimeter in size or when PSA levels are <10 ng/mL—when cancer may be more effectively managed or treated with localized therapy.
- They can be difficult in a clinical setting, especially for being time-consuming. They may present challenges for reproducibility of results.
- Patients may require multiple scans to evaluate all potential metastatic sites: Bone scans, CT, and/or MRI may be necessary.
For years, we have been able to detect prostate cancer recurrences with PSA. However, standard body and bone scans have been unable to determine the location of the cancer until the PSA level is excessively elevated (10 to 30 or higher). This makes it incredibly difficult to treat with confidence in the management plan at an earlier stage.
Axumin changes that by allowing detection and location at PSA levels of less than 10. Sometimes it may even detect at much lower levels, providing the advantage of time and accuracy to the treatment of the patient.
Axumin works by exploiting the fact that prostate cancers absorb amino acids at a much more rapid pace than normal cells. Axumin is made up of a radioactive tracer linked to an amino acid. Cancer cells absorb the amino acids more avidly than normal cells, so when Axumin is used, the radioactive tracer concentrates inside the tumor cells. When the patient is imaged, the areas that have a high concentration of the imaging agent signal the location of the cancer in the patient’s body.
According to Abhishek Solanki, M.D., assistant professor of radiation oncology, Loyola University School of Medicine, Chicago:
“Biochemically recurrent prostate cancer poses an important medical challenge. Currently approved anatomical imaging procedures have limitations in identifying the sites of recurrence of prostate cancer after definitive treatment, which can make decision-making difficult when assessing patients with biochemical recurrence. Newer imaging techniques, such as fluciclovine (18F) PET/CT, may provide actionable information for physicians in guiding appropriate patient management.”
Axumin helps with detection and localization of biochemically recurrent prostate cancer and represents a significant clinical breakthrough for managing these patients. The FALCON trial demonstrated that over 60% of management plans were changed when Axumin was used in the workup for patients with biochemically recurrent prostate cancer.
Indication
Axumin (Fluciclovine F18) injection is indicated for PET imaging in men with suspected prostate cancer recurrence based on elevated blood prostate-specific antigen (PSA) levels following prior treatment.
Clinical outcomes
Axumin is having a significant impact upon how clinicians treat recurring prostate cancer. In the LOCATE trial, 129/213 (59%) of patients had their clinical management revised after the results of Axumin PET/CT imaging were included in their diagnostic workup. 78% of these management changes were major – changing from a systemic non-curative therapy to salvage therapy, salvage therapy to systemic non-curative therapy or from salvage therapy to watchful waiting.
Within the remaining 22% of the patients who experienced a clinical management modification, 71% underwent a radiotherapy modification to include areas for therapy that would have otherwise not been treated.
In short, use of Axumin is a game-changer when it comes to optimal patient management of those with recurrent prostate cancer. Detection and localization at an earlier point in time is critical for developing the best possible management plan for the patient.
The patient-physician perspective
One of the major challenges with recurrent prostate cancer is being able to pinpoint it early. Cancers that have the ability to metastasize are the most dangerous for the patient. Prostate cancer that has spread to other parts of the body has a five-year survival rate of just 30%.
Axumin is vitally important from this perspective because it also helps physicians to determine where cancer is not. This signifies areas where treatment is not required, potentially saving the patient from the side-effects that aggressive treatments can bring.
Axumin also helps to detect whether the cause of elevated PSA is metastasized cancer or not. Sometimes recurrent disease is localized to the prostate or prostate fossa – aggressive treatments would be unnecessarily toxic to the patient in these cases.
In men who have received recent treatment with Lupron and Taxotere, an Axumin scan can hone in on any areas of cancer in the body manifesting persistent metabolic activity. This can be a sign that the cancer cells are still viable, despite the treatment. If these areas are limited in the patient, they may benefit from spot radiation or other treatments that are directed at residual disease. Again, this can be a less-traumatic approach for the patient than more aggressive treatments.
Interpretation of Axumin scans
Interpretation for PET/CT examinations using Axumin are different from standard FDG PET/CT imaging. Axumin specific training is available and is recommended for every interpreting physician. Below is a general guideline for interpretation, taken from Blue Earth Diagnostics’ Axumin site:
Prostate Bed (Prostatectomy)
Focal uptake, visually equal to or greater than bone marrow, in sites typical for prostate cancer recurrence is suspicious for cancer. If focus of uptake is small (<1cm), it may be considered suspicious if the uptake is visually greater than blood pool.
Prostate Bed (Non-prostatectomy)
Moderate focal asymmetric uptake, visually equal to or greater than bone marrow, is suspicious for cancer recurrence. If focus of uptake is small (<1cm) and in a site typical for recurrence, it may still be considered suspicious if the uptake is visually greater than blood pool.
- Diffuse and heterogeneous uptake visually greater than blood pool is suspicious for cancer.
- Diffuse and homogeneous uptake visually greater than bone marrow is suspicious for cancer.
Lymph Nodes (Typical sites for prostate cancer recurrence)
Uptake, visually equal to or greater than bone marrow, is considered suspicious for cancer. If node is small (<1cm) and in a site typical for recurrence, it may still be considered suspicious if visually greater than blood pool. If borderline visually, quantitation using a node (SUVmax) to background (marrow or blood pool; SUVmean) ratio may help.
Lymph Nodes (Atypical sites for prostate cancer recurrence).
Atypical sites may include: Inguinal, distal external iliac, hilar and axillary nodes. Mild, symmetric uptake is typically considered physiologic uptake, but if such nodal uptake is present within the context of other clear malignant disease, it may be considered suspicious for cancer recurrence.
Bone
Focal uptake, clearly visualized on Maximum Intensity Projection (MIP) or PET-only images, can be considered suspicious for cancer. A bone abnormality visualized on CT (e.g. dense sclerosis without uptake) does not exclude a metastasis. Alternative imaging, e.g.: MRI, NaF PET/CT or SPECT/CT bone scan, should be considered.
It is recommended to evaluate Axumin images with an “Inside-Out” approach: assess central areas of focal uptake in prostate/pelvis before assessing more peripheral areas.
Image interpretation is predominantly qualitative but, for areas of borderline increased uptake, an uptake ratio (SUVmax divided by SUVmean in background region) may be supportive.
Examples of background regions that be used include:
- Marrow: 1.5cm spherical VOI over normal L3 vertebra
- Blood Pool: 1cm diameter VOI in descending thoracic aorta extended over 2cm z-axis.
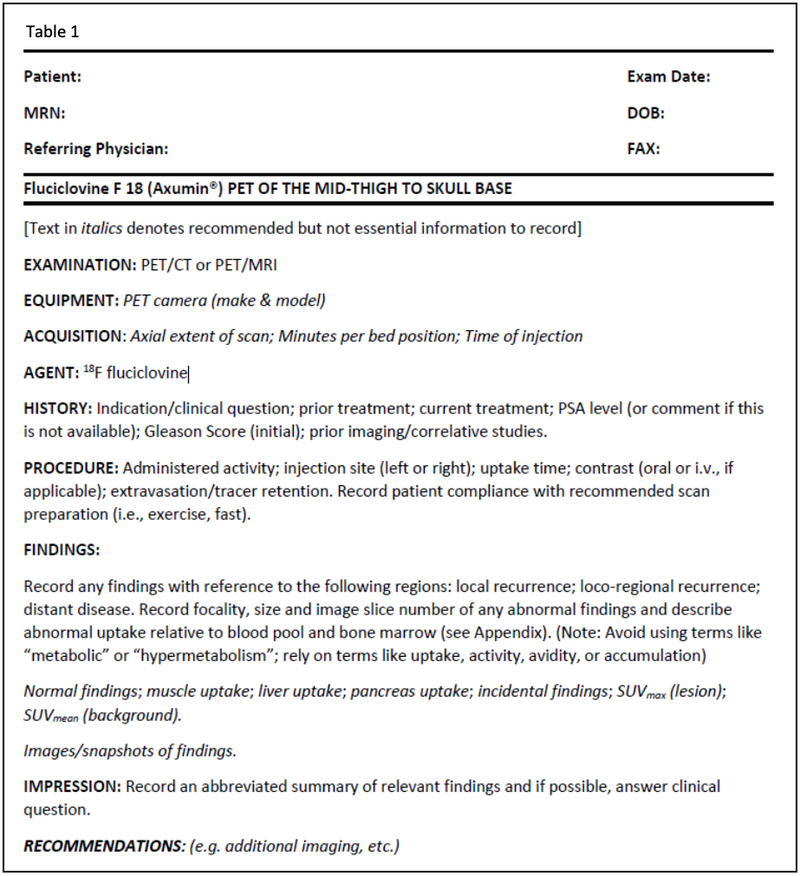
Reporting
A comprehensive Axumin PET/CT report should include:
-
- Information regarding the imaging equipment
- Dosing information
- Acquisition parameters
- Patient history
- Procedure findings
- Impression and any recommendations.
Final thoughts
Axumin (18Fluciclovine) is making a huge clinical impact on the detection and treatment of recurrent prostate cancer. An Axumin scan can:
- Detect cancer location at lower PSA levels
- Reduce the time spent on scanning
- Help physicians to hone patient treatment plans
- Help patients by avoiding unnecessarily aggressive treatments.
Axumin is both FDA and Medicare approved and is growing in availability among medical imaging facilities.




