MedAxiom recently held a webcast where the topic of Telehealth and Cardiology was explored in detail. The session was moderated by MedAxiom President, Dr. Jerry Blackwell, and featured a set of panelists with expertise in Telehealth.
The Sudden Shift to Telemedicine
The COVID-19 pandemic has caused upheaval in countless ways. For cardiology practices, this shift has involved a rapid and evolving move to Telehealth as a way to provide patients with care.
The move to virtual care is vital as a way to protect patients and staff. It’s also an essential way to mitigate the tremendous financial impact of the virus on practices. While no one wants to focus on the bottom line in a time like this, it is important for cardiologists to survive the crisis from a financial point of view, so they are strong and ready to treat patients after the urgent threat has passed.
Because this shift was primarily brought about due to the pandemic, there are no firm guidelines for payors or providers to follow. That said, there are best practices for cardiologists to use that are being developed as the pandemic unfolds.
Patient Triage
The first item to consider when you’re looking at Telehealth is who will require this service. During the MedAxiom webcast, the panel explained how breaking patients down into three categories helps classify the need. These “buckets” include:
Patients who must be seen in person: This group includes acutely ill patients who require urgent treatment and a face-to-face meeting.
Low-risk patients: This group involves patients whose conditions made it easy to reschedule treatment for a safer date. Moving their treatment three months out is a way to remove the risk to these patients and protect your staff.
Patients under active management: The third, and possibly largest, bucket is of patients who are under active management but that do not have acute symptoms. This group is ideal for Telehealth and can greatly benefit from what this service provides.
Even in these tumultuous times, it’s important for providers to remain vigilant about documentation. Something as simple as how you classify a patient can be important once we get through this period. Document why a patient was triaged into the category they are in and note the reasoning behind the decisions.
The Medicare Telehealth Guidelines: What We Know and What’s Changed
The rapid shift to Telehealth was accelerated when CMS issued a waiver in early March to drastically loosen and expand the ability for medical providers to offer virtual visits. The waiver removed requirements that have been in place, making it easier for more providers to quickly offer Telemedicine. Four key areas the waiver affected include:
Patient Setting: A central change in the wavier related to the setting for the visit. Under the new guidelines, patients can be consulted while at their home. This simple adjustment has far-reaching ramifications because it opens Telehealth to a much broader audience. The services that CMS covers remain the same and include established office visit codes that were used before the wavier.
Qualified Provider: The changes in the waiver also loosen and expand the qualified provider requirements relative to Telehealth. Now providers can be located at home if they are providing Telemedicine services. Earlier rules required the providers to be onsite at the clinic and did not cover consultations provided outside the office.
Patient Eligibility: Telehealth has always required that the patient have an established relationship prior to the Telemedicine visit. HHS has stated publicly that they will not conduct audits during this crisis, so you may be able to consult with new patients without a prior relationship. This can vary from payor to payor, so be careful with this expansion.
Technical Requirements: Prior to the waiver, strict HIPAA requirements were in place for the technology used to provide Telehealth service. Those rules have been loosened, and now visits can be provided using commercial technology such as FaceTime or Skype. Coding and reimbursement standards still apply if you are billing Level 3 or Level 4 visits, but the HIPAA restrictions have been greatly relaxed.
Telehealth Coding Guidelines
During the MedAxiom webcast, a core discussion topic was on the billing and coding of the Telehealth services. New laws, waivers, and changes within CMS have altered the way these codes can be used. For our current environment, there are three main divisions when it comes to Telehealth coding. These include telephone only, audio and video consultations, and an audio & video code related to emergency Telehealth coverage.
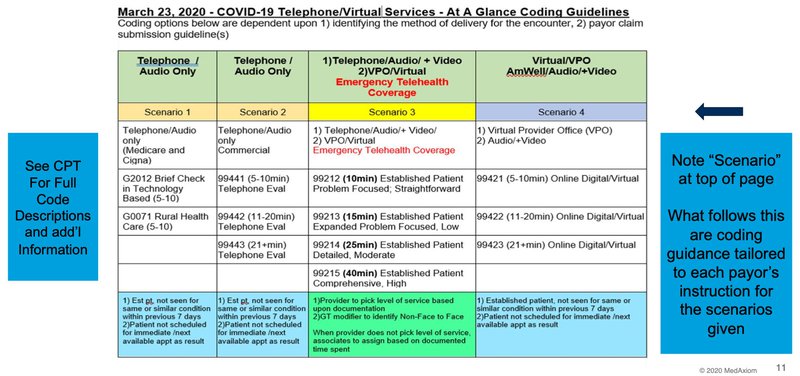
Telephone Only
There were existing codes for audio-only Telemedicine, but the problem is no one really paid for them. That has changed. When audio and video are not available, you can bill using these codes and be reimbursed. There is a division for rural vs. standard, and you bill according to the amount of time you spend with the patient.
Audio and Video
This set of codes covers audio and video Telehealth services and is intended for non-emergency cases. The codes vary depending on the amount of time you spend with the patient and have a 5-minute minimum.
Emergency Telehealth with Audio and Video
These codes are new and were created in response to the crisis. As with the standard codes, these are time-based and require a 10-minute minimum as opposed to 5. These codes allow you to bill standard E&M’s via Telehealth. In order to take advantage of the Telehealth codes, in an emergency setting, you MUST have audio and video. Billing for these codes requires a live, interactive, audio & video experience.
These are all time-based codes, and even though the rules are changing by the day, you must document your time. The Telehealth codes require patient consent that there may be a co-payment because this is an official visit. In 2020, due to the pandemic, you only have to ask for consent one time vs. each time you speak with the patients.
Are More Change Yet to Come Relative to the Waivers?
Changes are happening so rapidly that many Cardiologists and providers are wondering if more waivers or rule changes are yet to come. While payors are greatly expanding the acceptance of Telehealth codes, it could be that state or Federal mandates come down that require a blanket approval of Telemedicine services.
The requirement of video and audio is another area providers are closely watching to see if the minimums are relaxed. Full approval of audio-only calls would only expand the speed at which practices are providing Telehealth.
What’s Next for Telehealth and Cardiology
The rules, codes, and reimbursement standards around Telehealth are changing almost daily. Check the MedAxiom, SNMMI, and ASNC websites to get the latest on the rule relative to Telemedicine.
Regardless of how things ultimately settle, the barriers to Telehealth and servicing patients remotely are rapidly changing. Many cardiologists see this moment as a turning point. Once doors like this have been opened, it becomes very hard to close them, and ultimately this is good for patients.
What we do know is that as Telehealth becomes more standard, it will continue to change how cardiology practices operate. Instead of ignoring this trend and waiting for the storm to blow over, it’s wise to consider the role Telemedicine could play in your practice. The move to Telehealth can set your practice up for future success and keep your patients healthy and protected.