Artificial intelligence is developing rapidly in medicine, including in the field of cardiology.
If you’ve been to conferences in the last couple of years, you’ve probably seen presentations on some aspect of artificial intelligence. Quite simply, AI involves computer systems performing tasks that usually require human intelligence. They do this using techniques like deep machine learning and natural language processing.
AI is already seen in cardiology, performing tasks such as generating risk scores among patients. It is hoped that as AI develops further, it can help with improving the decision-making required on a daily basis, which has been proven to be subject to bias.
Here are some real ways that AI will change cardiology:
Counteract Unconscious Biases
Studies have proven that errors in decision-making can often come back to one of two types of bias. One of those is social bias, such as the categorizing of minorities or gender bias – in any case, this means that one group isn’t getting the same care as another.
In the case of cardiology, studies have shown that women tend to have a different experience than men, for example. Women are nearly twice as likely as men to die in the year following a heart attack, with a gendered difference in treatment being suspected in many cases.
The second type of bias that impacts errors in decision-making is “noise,” which means that decisions are impacted by irrelevant factors. For example, current mood, weather and the time since the last drink have all been found to impact decision-making.
The hope is that when AI is incorporated into daily decision-making in cardiology, it may help to counteract those unconscious biases. The caveat here is that the AI must be developed in such a way that it avoids bias. In some studies, AI has been found to amplify social bias in particular, especially in fields such as recruitment.
One solution to this is better sampling. AI “learns” from the data it is given, so if that data is skewed toward people who fit within a certain category, then it can build-in the bias.
AI in cardiology decision-making is strictly a tool to aid the final decision, not to actually make it. The cardiologist should still retain the last step in the control of the system and have the authority to change the outcome recommended by the algorithm, especially in cases where the decision could go wrong.
Provide Better Risk Prediction Models
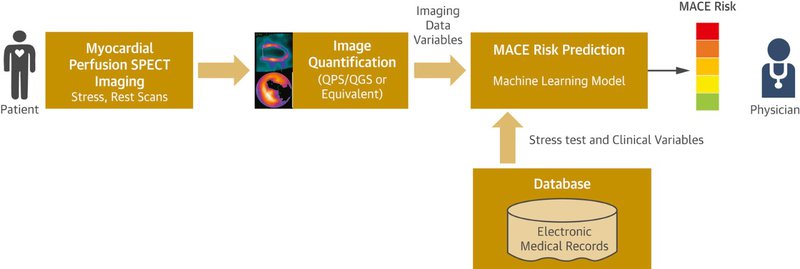
One exciting area undergoing development is the use of AI for patient risk prediction algorithms, where information is automatically extracted from medical imaging to offer better patient risk scoring.
Piotr J. Slomka, Ph.D., FACC, research scientist in the Artificial Intelligence in Medicine Program, Department of Medicine at Cedars-Sinai, and professor of medicine in-residence of the David Geffen School of Medicine, UCLA, is working with a Cedars-Sinai team to develop this.
From the Cedars-Sinai website: “Current research in the Slomka Laboratory focuses on developing innovative methods for fully automated analysis of nuclear cardiology data using novel algorithms and machine learning techniques, and on the development of integrated motion-corrected analysis of positron emission tomography (PET)/computed tomography (CT) angiography imaging.”
The image below illustrates how their proposed machine-learning model would allow prediction of the risk of major adverse cardiac events for a patient. This will be achieved by integrating clinical data with the imaging data.
Further information from the website states:
Specifically, the Slomka Laboratory aims to
-Develop new image-processing algorithms for fully automated analysis of fast-MPS. The algorithms will include better heart muscle detection by training with correlated anatomical data and a novel approach for mapping the probability of abnormal perfusion for each location of the heart muscle.
-Enhance the diagnosis of heart disease from fast-MPS by machine-learning algorithms that integrate clinical data, stress test parameters and quantitative image features.
-Demonstrate the clinical utility of the new algorithms applied to automatic canceling of the rest portion of the MPS scan when not needed.
ECGs and Non-invasive Glucose Detection
One factor that can put patients off proper glucose monitoring is the finger prick test. AI is set to change this by detecting hypoglycemic events from raw ECG signals.
The technology involves a non-invasive, wearable sensor which works with the AI to detect blood glucose. “…using the latest findings of deep learning they can detect hypoglycemic events from raw ECG signals acquired with off-the-shelf non-invasive wearable sensors.”
The results of pilot studies found that sensitivity and specificity was around 82%, comparable to Continuous Glucose Monitoring devices.
Automated Analysis of Cardiac Ultrasound
In November 2019, Ultromics received FDA clearance for their AI-drive echocardiography image analysis system, EchoGo Core.
“Traditionally, echocardiography has relied on the expert eye of clinicians, with years of experience, measuring the anatomical structures and identifying the disease, a potentially time-consuming and highly variable process. By automating the process and applying its AI analysis to look in greater detail at the scans, EchoGo enables clinicians to interpret echocardiograms efficiently and accurately and assists in their decision-making.
EchoGo uses AI to calculate cardiac ultrasound left ventricular ejection fraction (EF), the most frequently used measurement of heart function, left ventricular volumes (LV) and, for the first time for an AI application, automated cardiac strain.” (Source)
Faster Cardiac MRI Analysis
A recent study revealed that cardiac MRI analysis can be performed significantly faster and with similar precision to a human expert when using automated machine learning.
When analyzing heart function on a cardiac MRI scan, it takes humans an average of 13 minutes, whereas with AI, the analysis takes around 4 seconds. Many decisions in cardiology rely on accurate and timely analysis of MRI, so if AI can do this accurately, it can be a game-changer.
The study wasn’t used to demonstrate the superiority of AI over humans and was not used to analyze patient outcomes from clinical assessment. However, it highlights great future potential for improved efficiencies.
The Impact of AI on Cardiology
Artificial intelligence (AI) being developed for healthcare has been one of the biggest topics at just about all medical conferences the past two years, and the FDA has already started the market clearance of several AI algorithms for medical imaging and other aspects of cardiology.
Importantly, it is expected that AI will help to improve outcomes in cardiology. It can help to speed up decision-making and counteract any unconscious biases. We’re betting we’ll see many more AI developments in the medical field in the coming years.